Three ways digital transformation is accelerating the shift to preventive care
Jul 25, 2022 - Reading time 3-5 minutes
Amid a global pandemic, health systems are under more pressure than ever before. Hospital waiting lists have never been so long, with six million patients awaiting treatments in the UK [1], queues of 75 people awaiting each hospital bed in India [2], and similar backlogs being seen elsewhere around the world. The question is: how can today’s health systems relieve all this pressure, at scale, for good? Is a shift towards preventative care the answer?

According to a recent study by the World Economic Forum [3], the global economic impact of the five leading chronic diseases – which includes cancer, diabetes, mental illness, heart disease and respiratory disease – could reach US$47 trillion over the next 20 years. At the same time, the World Health Organization predicts that the global deficit of skilled healthcare professionals will reach 18 million by 2030 [4]. Clearly, even without the added chaos that a global pandemic brings, the burden of chronic disease – which also carries long-lasting impacts for patients’ social and psychological wellbeing as well as their physical wellbeing – will soon be too much for our health systems to handle.
All of this is why many healthcare organizations are now transitioning away from a model of intervention towards one of prevention: a model where resources are dedicated to detecting and forestalling medical issues before they have a chance to cause symptoms, develop into chronic diseases or trigger life-threatening events. For many parties across the healthcare ecosystem, from healthcare professionals to tech players and government bodies, the hope is that a preventive care model will be the solution to lifting the burden of chronic disease on our health systems, and ultimately, to delivering higher-value care that’s focused on enabling the healthiest outcomes.
Preventive care: three real-world examples
The concept of preventive care isn’t new – annual check-ups and immunizations are two examples of how preventive care has already been embraced for decades. But within the last few years, the digital transformation of healthcare has led to groundbreaking innovations that are rapidly accelerating the shift towards preventive care at scale. Here are three powerful examples:
1. Predictive analytics

Driven by the rise of Artificial Intelligence (AI) and the Internet of Things (IoT), many healthcare organizations now have algorithms at their disposal that can be fed historical as well as real-time data on their patients, so they can make meaningful, timely predictions about potential outcomes and treatment options. In many cases, these insights can inform decisions on both a cohort and population level.
For example, in cardiology, integrated diagnostics platforms enhanced with predictive analytics are now giving cardiology care teams the power to anticipate outcomes with greater accuracy, make faster clinical decisions, and (thanks to those insights) assign more effective treatment pathways to their patients, lowering the risk of unexpected events and interventions down the line.
2. Remote patient monitoring

Remote patient monitoring refers to a wide range of solutions that allow care teams to assess and sometimes even treat patients outside of conventional clinical settings, for more controlled management of chronic conditions, greater oversight over patients between visits, and fewer hospital readmissions. For example, remote cardiac monitoring solutions such as wearables and implantable devices can give care teams round-the-clock oversight on their patients from any location, collecting data on vital signs in real-time and flagging any signs of impending cardiac issues at the earliest opportunity. Solutions like these mean individuals with complex co-morbidities can finally emerge from cardiac events or procedures and go on to live independently, confident in the knowledge that their precious health data is being continually and securely communicated with their care teams.
3. Digital patient engagement
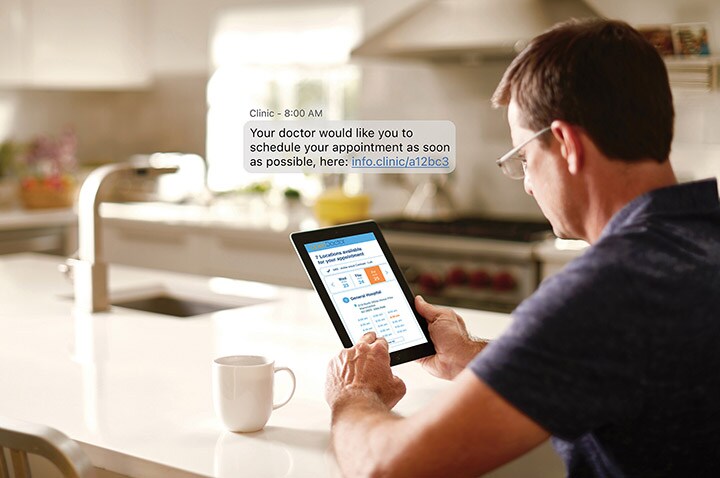
Digital patient engagement methods such as health-tracking apps and patient portals empower people to take a more active role in managing their health and wellbeing. They also help patients to maximize treatment compliance for existing conditions, and start dialogues with their care teams, for faster reporting of symptoms and greater access to information and advice. For example, pre-surgery health coaching apps help patients get in optimal condition before having elective surgery, so they can maximize the chances of shorter hospital stays while minimizing the chances of readmission. Collaborative patient-provider platforms are helping hospitals reduce the need for physical consultations – by as many as three per patient per year. And in oral health, electric toothbrushes coupled with health-coaching apps are helping both adults and children to monitor their brushing habits, learn more about the link between oral and systemic health, and stay engaged in developing healthy habits for life.
How can we keep up momentum for preventive care?
With around one in three adults being treated for complex chronic conditions globally [5], many of which have been identified as avoidable, lifestyle-related conditions, the need for a more preventive care model is all too apparent. The pandemic has spurred on much of the digital transformation that’s facilitating the shift to preventive care today – but these advances are long overdue. To make preventive care a success in all markets and alleviate the burden of chronic illness that’s been felt across the industry for years, we need to go further: breaking down the barriers between departments and specialists, eliminating the obstacles separating patients from caregivers, and bridging the boundary between healthcare settings and people’s homes.
Further reading
References
[1] British Medical Association. NHS backlog data analysis (bma.org.uk)
[2] The New Zealand Herald. India Covid-19 appeal: 'Up to 75 patients waiting for each hospital bed' - NZ Herald
[3] The World Economic Forum. WEF_Harvard_HE_GlobalEconomicBurdenNonCommunicableDiseases_2011.pdf (weforum.org)
[4] Clinton Health Access. There is a global shortage of nurses. COVID-19 is making it worse. - Clinton Health Access Initiative
[5] Science Direct. https://www.sciencedirect.com/science/article/pii/S2211335518302468








