For decades, healthcare has been delivered primarily in centralized facilities such as hospitals, enabling huge strides in the diagnosis and treatment of disease – but capturing only intermittent snapshots of our health, while not always being accessible to patients in remote or underserved communities. Today, thanks to digital health technologies, we see the rapid emergence of a new paradigm: one in which we can bring care much closer to the patient, whether that is virtually or physically, at home or in the community. Here’s why we believe distributed care is the future of healthcare.
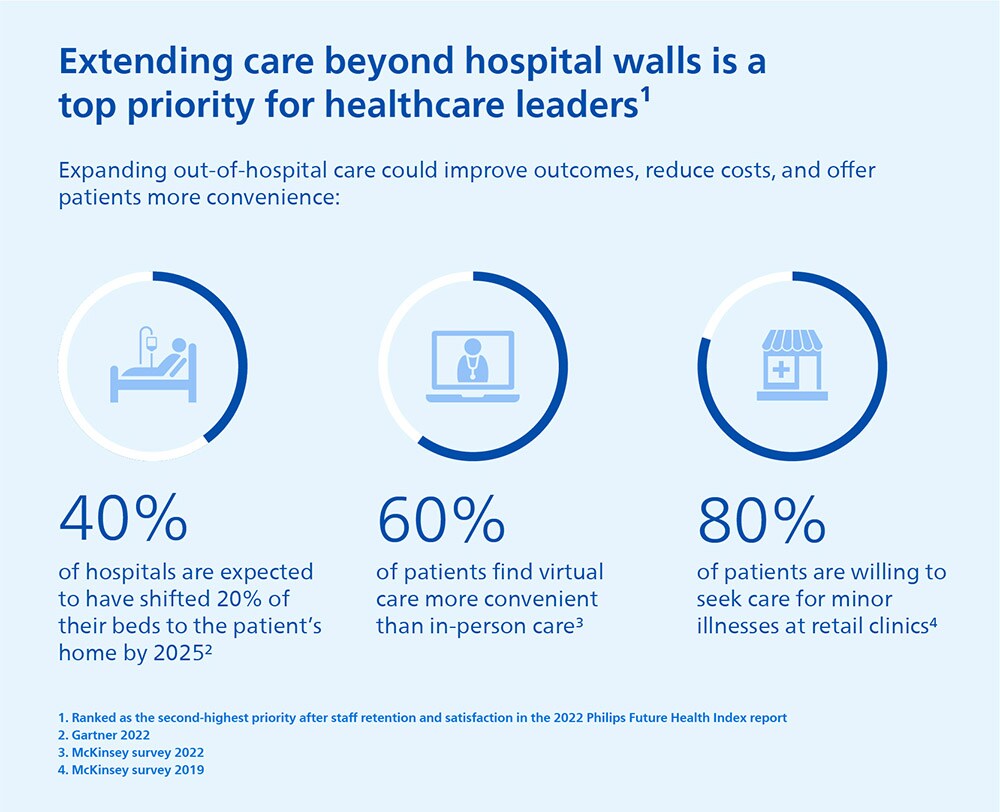
The trend towards out-of-hospital care was already well underway before the pandemic accelerated the adoption of digital triaging, telehealth, and remote patient monitoring. As this year’s Philips Future Health Index report reveals, healthcare leaders now view extending care delivery beyond the hospital as their highest priority after staff satisfaction and retention [1]. Like them, we believe that building more hospitals cannot be the only answer to meeting the growing demand for accessible and affordable care.
Distributed care flips the traditional hospital-centric care paradigm on its head. Instead of having patients come into a central location, distributed care brings care to the patient. Increasingly, we will see healthcare being delivered through a decentralized network of ambulatory clinics, retail settings, and home-based monitoring, coaching, and treatment. The glue that binds this network together is the end-to-end experiences of the patients it serves, throughout their care journey.
Why distributed care is the way forward
The reasons for this paradigm shift are more urgent than ever.
Health systems worldwide are coming under increased financial pressure, with healthcare expenditures taking an ever-bigger chunk out of countries’ GDPs [2]. In many countries, hospital care accounts for the largest share of those expenditures, amounting up to more than 1 trillion dollars in costs in the US alone [3]. There’s a growing awareness that in order for healthcare to remain affordable and sustainable, it needs to move into lower-cost settings whenever possible to address people’s health issues at a much earlier stage and ideally prevent them.
Adding to the challenge for hospitals is that they are not staffed to keep pace with the rising demand for care, while chronic conditions such as diabetes, heart disease, and cancer continue to proliferate. Globally, a shortage of 6 million nurses pre-COVID plus 4.7 million set to retire in the next few years has been exacerbated by an exodus from pandemic-related burnout, leading to an estimated shortfall of 13 million nurses by 2030 [4]. The outlook for physician shortages is equally concerning [5], prompting healthcare leaders to ask how they can divert care away from labor-intensive hospitals to more labor-efficient home and community settings.
Meanwhile, patients expect more digitalized healthcare experiences that don’t require them to spend precious time and money on travelling when – in some cases – they could just as well connect with their doctor remotely. Having become familiar with the benefits of telehealth during the pandemic, 60% of patients say they find virtual care more convenient than in-person care [6].
The pandemic also shined a harsh light on long-standing inequities in access to care in many parts of the world. In the 2022 Philips Future Health Index report, we see how this has kindled an increased sense of social responsibility among healthcare leaders to improve access to quality care for all patients, irrespective of location or background [7]. This is still a far cry from today’s reality in which half the world’s population lack access to the health services they need [8]. We can and must do better.
So what exactly does a more distributed and accessible healthcare system look like?
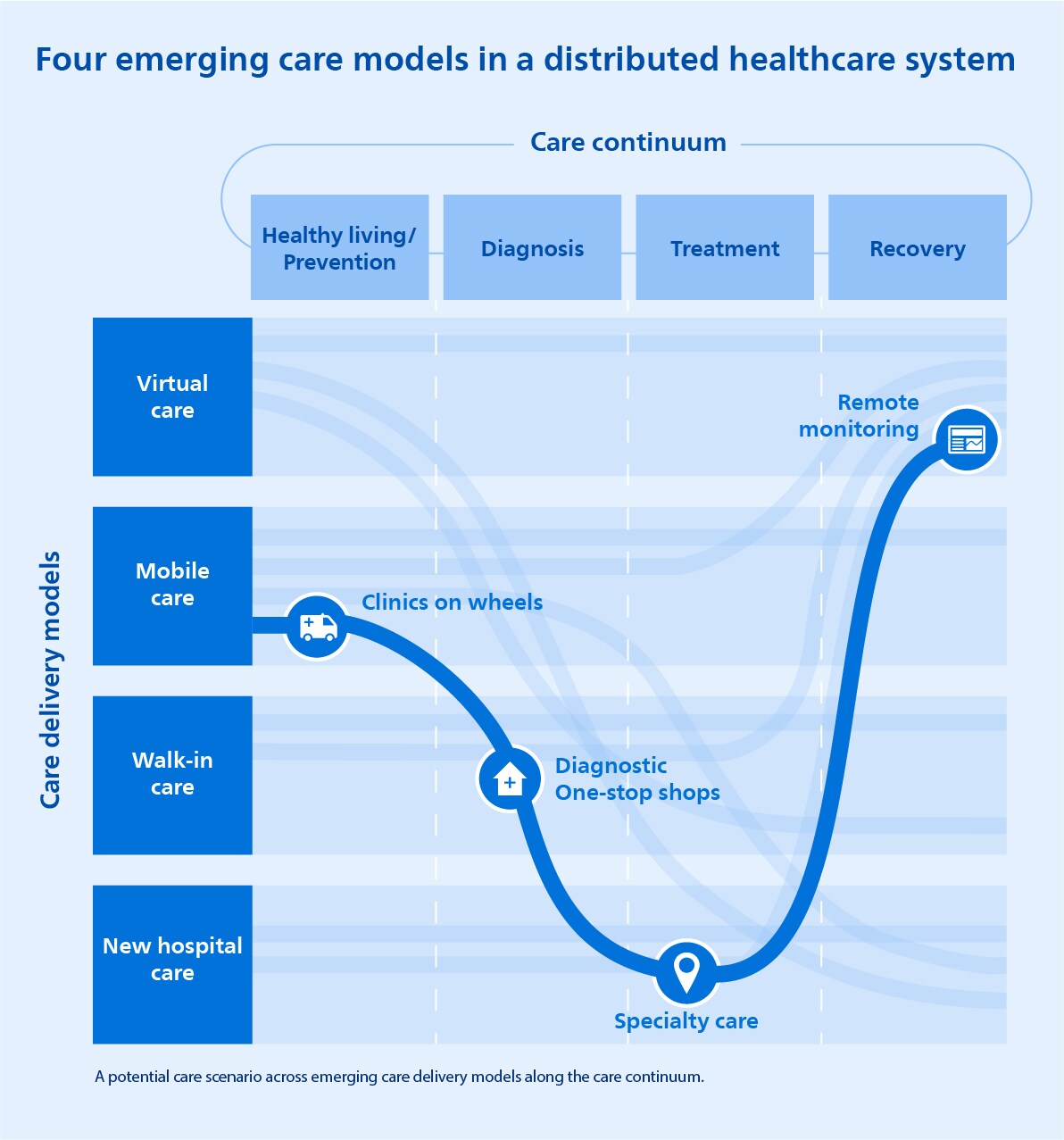
We find it helpful to distinguish between four care delivery models, as shown in the graph below that follows a patient’s care journey along different touchpoints. Let’s explore each model in more detail, starting with the one that has seen the most explosive growth in recent years: virtual care.
Connecting the hospital to the home with virtual care
When Australian healthcare provider West Moreton Health was faced with disproportionately high numbers of emergency department visits and potentially avoidable hospitalizations, they sought new ways of making quality care accessible for high-need, chronically ill patients.
Remote patient monitoring turned out to be a vital part of the solution. In partnership with Philips, West Moreton Health developed a virtual patient engagement program called MeCare, which uses home-based medical devices to collect patient-reported outcome data and biometric indicators including blood pressure and oxygen levels. Outcomes are reviewed in real time to proactively engage participants with personalized health coaching. Early results were significant, showing a 28% reduction of potentially preventable hospitalizations in chronically ill patients. West Moreton has since expanded the MeCare program to include more patients and more use cases, including COVID-19 monitoring, medication management, and mental health.
It’s a great example of how virtual care can offer healthcare professionals a window in patient’s day-to-day health. No longer do they have to rely on episodic measurements. They can now follow the patient’s health over time and provide ongoing care management, wherever that patient is located. In this case, that means patients in small rural communities in the West Moreton area also get to benefit, making the local healthcare system more equitable and inclusive.
Another way in which we are pioneering home-based patient monitoring is through wearable patches that support the early detection of heart rhythm irregularities to prevent (repeat) strokes. Such patches are becoming more and more unobtrusive, allowing patients to keep an active lifestyle while extending the line of sight of physicians from the hospital into the home. Add to that the power of cloud-based AI that can spot early signs of heart rhythm disturbances based on more than 20 million ECG recordings, and we can give care teams the insights they need to intervene preemptively.

Clinical-grade home-based ECG monitoring can also offer a boon to research. Rather than having patients come into a research site multiple times over the course of a trial, decentralized clinical trials equip patients with the tools to record and share data at home. Not only does this improve the patient experience, it can also help curb the attrition that often plagues clinical trials. Just as importantly, it can make clinical trials accessible for those who have traditionally been underrepresented. Typically, 70 percent of potential participants live more than two hours from trial sites. Decentralization broadens trial access to reach a larger and more diverse pool of patients, thereby contributing to better-quality outcomes that are more representative of the population at large [9].
Bringing specialist care to the heart of the community
Of course, not all clinical care or research can take place remotely. In-person interaction remains essential to many facets of healthcare. But that doesn’t mean it always needs to be tied to a fixed location that requires patients to travel. What if care moved out on wheels to travel to patients instead?
That’s exactly the premise of mobile healthcare services. For example, during the first wave of the COVID-19 pandemic in India, we launched a first-of-its-kind mobile Intensive Care Unit (ICU), equipped with nine beds, which can be deployed in one day to rapidly increase ICU capacity where it’s needed and enhance community outreach. Such highly flexible solutions can help mitigate the impact of future disasters and pandemics to improve access to care and avoid hospitals from being overrun.
As another example of mobile care, we have been piloting the use of health trucks in the Japanese city of Ida, bringing on-demand primary care services to patients in underserved communities where qualified healthcare professionals are in short supply. Coupled with telehealth facilities, mobile health trucks allow patients to connect with a remote clinical expert. The clinical expert, in turn, can offer virtual guidance to assist a local healthcare worker in using advanced mobile equipment such as a handheld ultrasound scanner.
While much work remains to be done to scale the use of such mobile diagnostic solutions, we believe they hold great promise for the future. Enhancing them with AI would make it even easier for local healthcare workers to acquire the right images and then interpret them correctly. That’s why we’re excited to be working with the Bill & Melinda Gates Foundation on an AI-based ultrasound application that will be designed to help nurses in low- and middle-income countries identify potential pregnancy complications at an early stage, thereby giving expecting moms a better chance of bringing a healthy child into the world. Especially in areas where the nearest hospital may be many miles away, mobile healthcare solutions can make a real difference right in the heart of the community.

Lowering the barrier to access with walk-in care
In lockstep with the rise of virtual and mobile care, we will see more and more healthcare services being delivered in walk-in settings such as department stores, shopping malls, gyms, and airports. During the pandemic, pop-up clinics have played a pivotal role in relieving the strain on overwhelmed healthcare systems by providing testing and vaccinations on a large scale [10]. There are many other routine exams and medical procedures that could also be delivered in community-based settings to relieve hospital resources, improve access to care, and support early detection and diagnosis of disease.
For example, the NHS in England is planning to build one community diagnostic center for every 300,000 people – amounting to up to 150 diagnostic hubs. As the vision video below shows in more detail, these “one-stop shops”, which are located away from hospital sites closer to patients’ homes and often on the high street or in retail locations, will provide specialist services for cardiovascular patients, people with cancer, and those with respiratory illnesses – supported by expert teleconsultations where needed.
Similarly, in the US, where people in rural or remote areas make up one fifth of the population, we have designed virtual care stations that allow patients and providers to connect remotely through a secure, clinical-grade environment. In addition, we are bringing innovations in image-guided therapy closer to patients through out-of-hospital settings such as office-based labs or ambulatory surgery centers, which can perform routine procedures at lower cost while offering patients greater convenience.
The future of hospital care in a distributed network
Where does this leave the role of the hospital?
As healthcare becomes increasingly distributed, hospitals will continue to play a critical role. But it will be different from the one they have played traditionally. Most hospitals will no longer provide all services under a single roof. Instead, they will focus on delivering a narrower set of specialized services and acute care, while simultaneously taking a more prominent role in managing population health in the community and at home. Hospitals without walls will emerge, serving both as a central physical hub and as an orchestrator of a wider ecosystem of care.
At the same time, hospitals will be forced to operate much more efficiently to keep delivering high-quality care with increasingly scarce resources – all while offering a seamless patient experience before, during, and after hospital visits, taking an end-to-end view that spans the entire continuum of care. It is a truly transformational challenge, which we will explore more deeply in our next blog post.
The promise of anytime-anywhere care has been a long time coming. There’s no going back now. The future of healthcare doesn’t center around a location – it centers around the patient, wherever they live, and however they can best access the care they need in the moment.
References
[1] https://www.philips.com/a-w/about/news/future-health-index/reports/2022/healthcare-hits-reset
[2] https://www.oecd.org/els/health-systems/health-expenditure.htm
[3] https://www.fastcompany.com/90546914/the-1-trillion-quest-to-bring-hospital-care-to-your-home
[4] https://www.weforum.org/agenda/2022/01/health-care-nurses-attrition-mental-health-burnout/
[5] https://www.aamc.org/news-insights/press-releases/aamc-report-reinforces-mounting-physician-shortage
[6] https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality
[7] https://www.philips.com/a-w/about/news/future-health-index/reports/2022/healthcare-hits-reset
[8] https://www.weforum.org/agenda/2019/09/half-of-the-world-s-population-lack-access-to-essential-health-services-are-we-doing-enough/
[9] https://www.mckinsey.com/industries/life-sciences/our-insights/no-place-like-home-stepping-up-the-decentralization-of-clinical-trials
[10] https://www.medicaldirector.com/news/future-of-health/2022/02/are-pop-up-clinics-the-future-of-healthcare
Share on social media
Topics
Author

Henk van Houten
Former Chief Technology Officer at Royal Philips from 2016 to 2022

Sean Carney
Former Chief Experience Design Officer at Royal Philips from 2011 to 2022

